Good Laboratory Practice (GLP) is a set of criteria used to ensure quality assurance in non-clinical studies. GLP principles are concerned with the organisational processes by which studies are planned, performed, monitored, recorded, reported and archived. These guidelines support the integrity, reliability and traceability of safety data used for regulatory submissions.
GLP is commonly applied in the pharmaceutical industry, where it guides pre-clinical stages of drug development and clinical pharmacology. However, good laboratory practices also apply outside pharmaceuticals, including the safety testing of food additives, packaging, chemicals and medical devices.
What is the purpose of Good Laboratory Practices?
In clinical pharmacology, the main aim of GLP is to ensure that all drugs being tested during non-clinical stages follow a controlled and consistent quality management process before approval for human use in clinical trials.
This helps ensure that stringent safety standards are followed before First-In-Human testing, reducing potential risks to participants. GLP also makes sure that written procedures are followed, limiting external variables that could affect the reliability of data used to approve drugs for clinical research.
The Importance of Good Laboratory Practices
The importance of good laboratory practices lies in their ability to ensure that non-clinical safety studies are transparent, reproducible and scientifically sound. Regulatory bodies rely on GLP-compliant data to determine whether a product is safe to progress to human trials. Without GLP, the safety profile of a product may be considered incomplete or unreliable.
GLP supports:
- high-quality, traceable safety data
- consistent study conduct
- accurate reporting and archiving
- confidence in pre-clinical results used for regulatory decision-making
GLP Guidelines: What Do They Cover?
In order to comply with GLP, it is important that studies are conducted in line with the following guidelines.
Personnel
Prior to the research taking place, there must be an appointed Study Director whose responsibility is to conduct and oversee the study’s GLP compliance and budget. This must be accompanied by a separate Quality Assurance Unit (QAU) that is independent of the testing facility organisation.
This ensures that the study has dedicated personnel to monitor and manage GLP compliance.
Study plan
The study plan should outline how the study will be conducted, including time schedules, stages of work, and the methods and materials used. Sometimes referred to as the study protocol, the plan must undergo approval and review before the study can begin.
The study plan is then reviewed by the Quality Assurance Unit, which assesses its compliance with Good Laboratory Practice.
Standard operating procedures
Standard operating procedures (SOP) outline step-by-step instructions that provide methods for carrying out routine operations in laboratory and clinical settings. These procedures help improve efficiency, quality output and communication.
SOPs must outline all Good Laboratory Practices, giving staff clear instructions to follow. This should cover:
- Equipment guidelines
- Testing items
- Record keeping, reporting and storage
- Biological test systems
- Testing and analysis procedures
- Computer system guidelines
- Quality assurance procedures
Facility, equipment and handling
Facilities and equipment must be organised, maintained and labelled appropriately. This helps improve safety and workflow, and ensures all personnel understand laboratory procedures when using central laboratory facilities.
Facility workers must keep records of:
- date of receipt and expiry for test and control items
- storage conditions
- identity, purity, composition and stability of materials
- quantity received and used
Study reports
The study director is also responsible for the study report, an essential part of medical writing. The report must detail:
- How the study was conducted
- any deviations from the SOPs or study plan
- results of the research
- a critical scientific discussion
- a GLP Compliance Statement
Study records
According to Schedule 1 of the UK GLP Regulations, study data must “be retained in archives for the period specified by the appropriate regulatory authorities”. This includes:
- study plan
- raw data
- samples and reference items
- final report
These records support the QAU and regulatory inspections.
Good Laboratory Practice Examples
Common examples of GLP principles include:
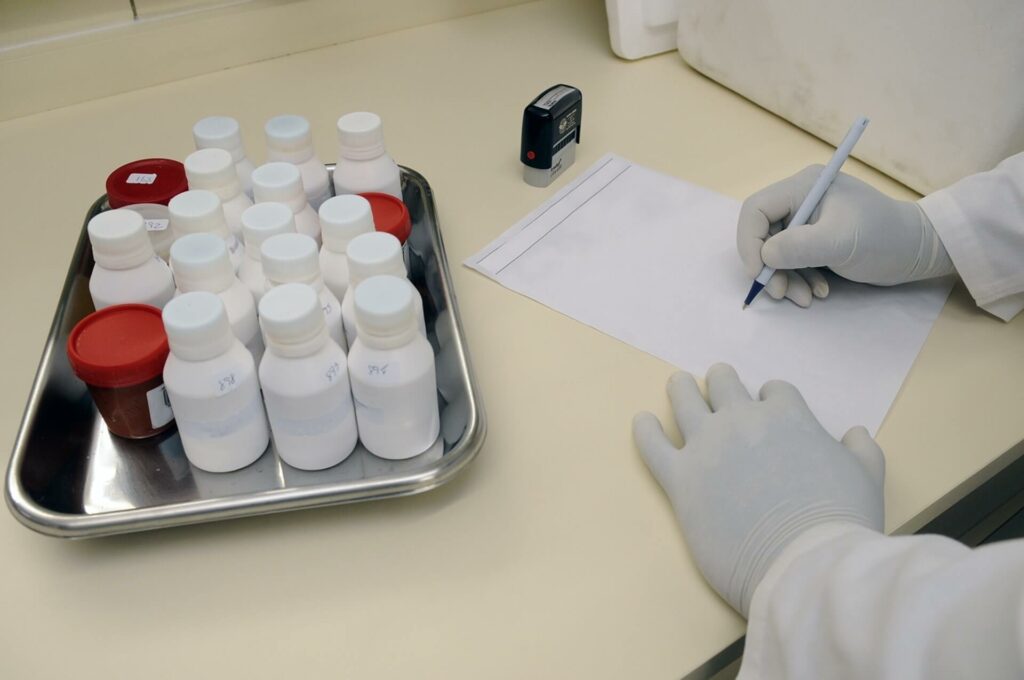
- Wearing PPE
- Communicating frequently with all personnel in the laboratory
- Attending to unfamiliar smells or materials
- Cleaning equipment regularly
- Labelling workspaces
- Avoiding working alone
- No food or drink
When is GLP required?
GLP regulations are applied in the UK, the US and the EU. They are required for non-clinical safety, toxicology and pharmaceutical studies that have been proposed for human applications.
These guidelines were established by the Organisation for Economic Co-Operation and Development (OECD). GLP is only required in non-clinical studies and testing, and does not apply to later clinical stages of research.
Following this, clinical stages of research are governed by Good Clinical Practices (GCP), which are intended to keep human participants safe during the study process.
Often, GLP is applied where it is not necessary. It is important to distinguish the differences between the different practice regulations required at different stages of clinical research.
GCP vs GLP
The main difference between GCP and GLP is their applications. Good Laboratory Practice (GLP) applies to pre-clinical drug safety testing, whereas Good Clinical Practice (GCP) is applied across the whole clinical research process.
GCP and GLP are both inspected by the Food and Drug Administration (FDA), used to ensure safety and quality throughout the non-clinical and clinical research process.
CRO services
As a full service CRO, we offer integrated central laboratory services to support clinical development needs. We are experts in regulatory affairs, helping support your strategy with GLP and other regulatory compliance processes to aid fast study approvals. Speak to our team to get started.
Good Laboratory Practices FAQS
Why are Good Laboratory Practices important?
The importance of GLP lies in its ability to guarantee that non-clinical safety studies are conducted to a high and consistent standard. Regulators depend on GLP-compliant data to determine whether a drug or product can progress safely into human research, reducing risks to participants and preventing costly delays.
When is GLP required?
Good Laboratory Practices are required whenever non-clinical safety data is intended for regulatory submission. They apply to early-stage research conducted on cell or animal models before human involvement.
What is the difference between GLP and GCP?
The main difference between GLP and GCP is the stage of research they govern. GLP regulates the quality and integrity of pre-clinical data, whereas Good Clinical Practice (GCP) sets the standards for clinical trials involving people.
What are examples of Good Laboratory Practices?
Good Laboratory Practice examples include wearing PPE, following SOPs, correctly labelling samples, maintaining clean workspaces, recording the handling of test items and ensuring equipment is serviced regularly.